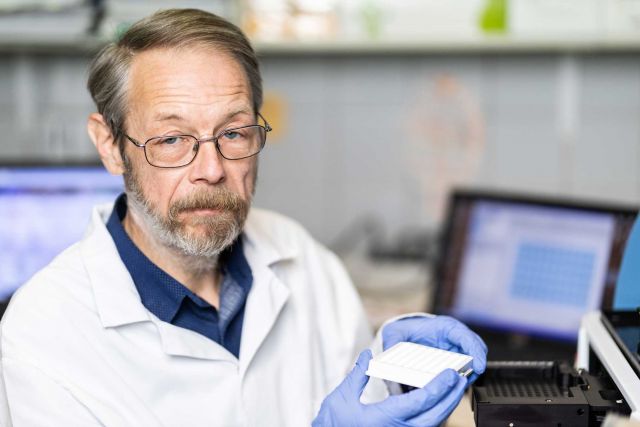
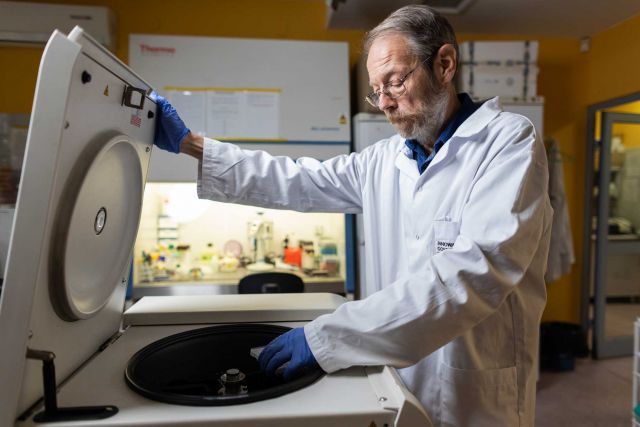
Principal Investigator
:
Prof. Dr hab. n. med. Maciej Cedzyński
Institute of Medical Biology of the Polish Academy of Sciences
Panel: NZ6
Funding scheme
: OPUS 6
announced on
16 September 2013
Haematological and lymphatic malignancies, often referred to as haematological or blood cancers, pose a serious threat to life. Some of these diseases (e.g. multiple myeloma or various lymphomas, which were the subject of this project) are treated with high-dose chemotherapy aimed at destroying the bone marrow that produces abnormal blood cells. Following chemotherapy, patients receive a transplant of healthy hematopoietic stem cells, either their own (isolated from the blood with special techniques) or sampled from a donor (which is known as a bone marrow transplant). However, such patients often die from infections, particularly common after chemotherapy, which also kills blood cells that produce antibodies or directly eliminate pathogens (e.g. phagocytes), before they go back to normal levels and activity after the transplant. Our research aimed to estimate the impact of selected immune factors circulating in the blood, which are not related to but sometimes cooperate with cells, on patient health, and in particular the risk of cancer and post-chemotherapy infections. We focused mainly on the molecules that recognize disease-causing bacteria, opsonize (coat) them, thus marking them for elimination by phagocytes, and activate the complement system (a complex system of many proteins that circulate in the blood), which removes pathogens by destroying their cell envelopes.
 Photo by Michał Łepecki
Our research showed that:
Photo by Michał Łepecki
Our research showed that:
- a deficiency of mannose-binding lectins (MBL) may be associated with a higher risk of multiple myeloma. The deficiency does not affect the patients’ risk of infection during the first weeks following chemotherapy and bone marrow transplant (during hospitalization), but may lead to enhanced susceptibility to serious, life-threatening infections at a later date when the normal phagocyte activity is restored. Accordingly, the effective elimination of many pathogens requires both active MBL (opsonization) and phagocytes that eliminate the lectin-coated bacterial cells
- certain variants of the MBL2 gene (which codes for the MBL protein) may be associated with a lower risk of various lymphomas.
- certain variants of the FCN2 gene (which codes for ficolin-2, a protein with properties similar to those of MBL) may be associated with a higher risk of various blood cancers.
- Certain variants of the MASP1/3, MASP2 genes (coding for enzymes that create complexes with MBL and ficolins and are important for the complement activation process) and the FCN3 gene (ficolin-3) may be associated with a higher risk of hospital infections.
- high pre-chemotherapy serum concentrations of MBL and MASP-2 may predict a higher risk of hospital infections.
- the serum levels of the immune factors under study show significant fluctuations (samples were collected immediately before chemotherapy, before the hematopoietic cell transplant, and 2-3 times more at weekly intervals). Their changes depend on the factor and the type of chemotherapy. A systematic increase of MBL level, increase, followed by a decrease of MASP-2 concentration, as well as a decrease and subsequent increase of the levels of ficolin-1, ficolin-2 and ficolin-3 were usually observed. The concentration of these proteins normally returned to baseline levels c. 3 months after the transplant. For a complex of two MBL-like proteins, known as CL-LK, we observed a relatively low reduction in serum level after chemotherapy, followed by values close to the baseline concentration in subsequent samples.
- the studied factors recognize the cells of some bacteria present in clinical samples isolated from patients and identified as infectious pathogens (e.g. staphylococci).
 Photo by Michał Łepecki
The impact of the polymorphism of some of the studied genes on disease risk and the differences in the levels of some proteins between patients and healthy subjects, as well as patients with and without complications, and their fluctuations, which often correlated with changes in cell count and/or biochemical inflammation marker levels, suggest that they could potentially be used as so-called auxiliary markers.
Photo by Michał Łepecki
The impact of the polymorphism of some of the studied genes on disease risk and the differences in the levels of some proteins between patients and healthy subjects, as well as patients with and without complications, and their fluctuations, which often correlated with changes in cell count and/or biochemical inflammation marker levels, suggest that they could potentially be used as so-called auxiliary markers.
Realisation of the project was possible thanks to cooperation with Medical University of Łódź, Institute of Oncology (Gliwice Branch), Hematology and Transfusiology Institute (Warsaw), University of Silesia (Katowice) as well as Aarhus University (Denmark) and Tokai University (Japan).
Project title: Factors specific for lectin pathway of complement activation in patients with haematological malignancies, receiving autologous haematopoietic stem cell transplantations
Prof. Dr hab. n. med. Maciej Cedzyński
Graduate of the Faculty of Biology and Earth Science of the University of Łódź. In 2021, he was awarded the title of professor in medical and health sciences. He heads the Laboratory of Immunobiology of Infections at the Institute of Medical Biology of the Polish Academy of Sciences, which focuses on studying the lectin pathway of complement activation and its role in human disease, as well as the mechanisms of interaction of collectins and ficolins with bacterial and cancer cells. He is a member or the Committee for Immunology and Aethiology of Human Infections of the Polish Academy of Sciences.